Our Surgical Weight Loss Team
At the South Bay Metabolic and Weight Loss Institute we have harnessed the collaborative power of multiple specialists and subspecialists into one comprehensive team of expert surgeons.
For more than 25 years, we’ve provided quality care for our patients while paving the way for future medical innovations. Our expert surgeons have performed countless weight loss procedures such as the gastric bypass and sleeve gastrectomy. We have pioneered the use of minimally-invasive techniques and key-hole surgery. Patients benefit by experiencing less pain, have very small scars, and recover faster.
Check out the information below.
- To improve general health, quality of life, and live longer
- Reduce risks for other surgical procedures such as total joint, hip or knee replacement
- To avoid heart disease & stroke
- Feel better, look better
- Improve mobility
- Alleviate and potentially cure diabetes and other medical problems
Someone who has been overweight and struggling with weight loss. Someone trying to live better and healthier, but is having difficulty losing weight. A person with a BMI (Body Mass Index) 35 or greater. New or ongoing health problems related with being overweight such as:
- Pre-diabetes
- Diabetes
- High blood pressure
- High cholesterol
- Sleep apnea
- Polycystic ovary syndrome (PCOS)
- Osteoarthritis
A decision for Surgical Weight Loss is never easy. When that choice becomes a life-changing event we are here to help. With more information available to you, this will help you to make the right decision best for YOU. A new you will require substantial effort, both mentally and physically, and we will be by your side.
Our partnership with Torrance Memorial Medical Center and Providence Little Company of Mary means that your surgery will be conducted at premier Center of Excellence facilities. This is a national accreditation standard given only to top performing hospitals. Both hospitals are equipped with state-of-the-art technologies enabling our surgeons to safely perform the latest procedures in weight loss surgery.
Additionally, Torrance Memorial has been selected as a Bariatric Surgery Center of Excellence by Blue Cross of California and Aetna networks.
Please, Join Us and Experience the South Bay Surgeon Difference!
Bariatric Surgery Specialists
Bariatric (weight loss) surgery can be extremely helpful not in just weight loss but in regaining better health and wellness. For example, bariatric surgery has been medically proven to improve your quality of life and INCREASE your lifespan. Let us help you live better, healthier, and longer!
Bariatric Surgery Q & A
Obesity is a progressive condition that is life-threatening. People who are overweight or obese have an increased risk of developing Type 2 diabetes, heart disease, high blood pressure, stroke, sleep apnea, respiratory issues, gallbladder disease, osteoarthritis, infertility, depression, and certain types of cancer. It’s currently estimated that obesity results in around 400,000 deaths every year. In cases of severe obesity, it’s difficult to treat with just diet and exercise. Only about 1 out of 20 obese people find success this way. This is where we can help.
Weight loss surgery is best suited for those who have tried and exhausted multiple weight loss strategies and exercise programs but remain overweight with multiple medical problems or still obese.
Bariatric surgery, otherwise known as weight loss surgery, works by greatly restricting the stomach’s ability to hold food and by changing the process of digestion. This will restrict the ability to eat large volumes of food and change your body’s desire to eat. In certain surgical procedures it decreases how much food (calories and nutrients) is being absorbed into the body.
Bariatric surgery is only the start of the weight loss journey. This is a life-long process of healthy living. Patients have to be fully committed to making lifestyle change – eating healthy and exercising regularly. If a person is dedicated to losing weight and getting healthy, they’ll maximize the benefits of weight loss surgery.
Laparoscopic Bariatric Surgery
Laparoscopic surgery utilizes a camera and long slender instruments placed within the abdomen to perform the operation. This is in contrast to the traditional open incision, which is a large incision made on the abdomen.
Because of the smaller incisions used with laparoscopic surgery, pain after surgery is less and the recovery is faster. In addition, with the smaller incisions, the body perceives less injury and less stress hormones are released that can be detrimental to healing.
Mortality and complication rates are the same or better with laparoscopic surgery compared to traditional surgery. The incidence of wound infections and hernias after laparoscopic surgery is negligible. This is in comparison to open surgery with hernia rates as high as 20% and wound infections of 13%. There is also a decrease in scar tissue formation with less risk of bowel obstruction in the future.
Laparoscopic weight loss surgery provides comparable weight loss and similar resolution of co-morbidities to the traditional open surgery (the same operation is done). The surgical “leak” rate (< 1%) and risk of blood clots (0.5-1%) are equivalent. Whenever an operation is attempted laparoscopically there is always a risk of not being able to complete laparoscopically and an open incision may need to be made. The risk of conversion to the open method is very low.
Diabetes and Bariatric Surgery
Diabetes Mellitus (DM) is a chronic disease of having irregular blood sugar levels. Insulin is produced in order to get sugar (or glucose) from the blood stream into the body’s cells where it is then utilized. Diabetes causes this system to not work properly. Type I DM is genetic, and has to do with inadequate insulin production. Adult Onset or Type II DM is often associated with weight gain. This is the most common type of diabetes, affecting 90-95 % of Americans with diabetes.
In Type II DM, also called non-insulin dependent DM, the glucose is constantly high in the blood stream and the pancreatic cells producing insulin cannot keep up or become overstimulated so they are no longer responding to the high blood glucose level. The result is the blood glucose levels remain high, and the body’s cells are not able to utilize the glucose.
Risk factors for Type II DM include increased body fat, especially fat that is carried centrally in a person’s mid section (central obesity). There may also be a genetic component to the development of Type II DM.
There are prediabetic states; which may mean a person is predisposed to developing Type II DM. The HgbA1c is a blood test that can be done to check for diabetes. Typically levels above 6 is considered diabetic, up to 5.5 is normal. Levels between 5.5 and 6 indicate a predisposition to Type II DM. A glucose tolerance test is another way blood test to diagnosis diabetes.
Metabolic Syndrome describes a cluster of conditions that are associated with an increased risk of heart disease, stroke and diabetes. The conditions include elevated blood pressure, glucose and cholesterol levels, along with central obesity.
Type II DM is a progressive disease and affects the nerves and blood vessels throughout the body.
| System or Organ | Complication |
| Circulatory System |
|
| Nervous System |
|
| Digestive System |
|
| Immune System |
|
| Kidneys |
|
| Eyes |
|
When obese patients lose weight, Type II DM often will be easier to control and in some cases, resolve. Bariatric surgery has been used as a tool to help patients stay on track with proper eating habits and lifestyle changes that lead to long term weight loss and improved health.
As more and more bariatric surgery is being done, we know now that bariatric surgery can actually cure Type II DM.
| Bariatric Surgery | Cure Rate for Type II DM |
|---|---|
| Roux-en Y Gastric Bypass | 83 %1,2 |
| Sleeve Gastrectomy | 80 %3 |
| Adjustable Gastric Band | 48 %2 |
The gastric bypass has a cure rate of 83% for Type II DM, 60 % with the sleeve gastrectomy, and 35 % with the adjustable gastric band.
Blood sugars are controlled very early after surgery, before weight loss has occurred, even before patients leave the hospital. Some of this has to do with the initial postoperative diet which consists of a very low calorie, low carbohydrate liquid diet. Also, as a person’s weight drops, their sugars often lower because of the lower fat mass.
What is unique with the gastric bypass is that the first portion of the small intestine (the duodenum and proximal jejunum) is bypassed. Because food is no longer going into that first part of the intestines there is a change in the hormone balance released by the gut that allows better control of diabetes. We do not yet know how this works but some of the hormones involved include Leptin (which suppresses appetite) and gut peptide hormones. In addition, there may be some improvement in insulin sensitivity by the body’s cells so glucose is better utilized.
- Schauer PR. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Annals of Surgery 2003;238: 467-482.
- Buchwald H. Bariatric surgery: A systematic review and meta-analysis. JAMA 2004;292: 1724-37.
- Leonetti F. Obesity, type 2 diabetes mellitus, and other comorbidities. A prospective cohort study of laparoscopic sleeve gastrectomy vs medical treatment. Arch Surg. 2012;147(8): 694-700.
Gastrointestinal surgery may be the next step for people who remain severely obese after trying nonsurgical approaches. Candidates for surgery:
- BMI of 40 or more
- BMI 35 or more with life-threatening obesity-related diseases such as diabetes, severe sleep apnea, or heart disease
- Obesity-related physical problems that interfere with employment, walking, or family function.
- No endocrine cause of obesity
- Absence of drug or alcohol problems
- Nonsmoker
- No uncontrolled psychological conditions
- Dedicated to life-style change and follow-up
If you fit the profile for surgery, answers to the following questions may help you decide whether weight-loss surgery is appropriate for you. Are you:
- Unlikely to lose weight successfully with nonsurgical measures, including medically supervised programs?
- Well informed about the surgical procedures and the effects of treatment?
- Determined to lose weight and improve your health?
- Aware of how your life may change after the operation (adjustment to the side effects of the surgery, including the need to chew well and inability to eat large meals)?
- Aware of the potential for serious complications, dietary restrictions, and occasional failures?
- Committed to lifelong medical follow-up?
Remember: Not every sufferer is a candidate for surgery. Bariatric surgery is an elective operation and the benefits of surgery must outweigh the potential risks of surgery. There are no guarantees for any method, including surgery, to produce and maintain weight loss. Once the decision has been made to pursue surgery, treatment does not end with the operation. That is merely the beginning. Success is possible only with maximum cooperation and commitment to behavioral change and medical follow-up—and this cooperation and commitment must be carried out for the rest of your life.*
The Next Step
Once your decision has been made to pursue surgical intervention for long-term weight loss and your medical doctors have deemed it safe you will need to be evaluated by the Bariatric team. A detailed and extensive medical and diet history as well as physical examination will be performed. There may be several tests that will need to be done in order to assess your surgical risks for complications. These may include but are not limited to Echocardiography, Stress tests, pulmonary function studies, sleep apnea studies, and endoscopy. A psychological evaluation and dietary consultation is required of all surgical candidates. In addition, you will meet with your surgeon for a comprehensive discussion of which surgery would be most appropriate for you. There will also be classes and support group meetings to attend in preparation for surgery.
BMI
Calculate Your Body Mass Index
Body mass index (BMI) is a measure of body fat based on height and weight that applies to adult men and women.
- Enter your weight and height using standard or metric measures.
- Select "Compute BMI" and your BMI will appear below.
Categories: Underweight
- Underweight = <18.5
- Normal weight = 18.5 ‐ 24.9
- Overweight = 25 ‐ 29.9
- Obesity = BMI of 30 or greater
What Are the Surgical Options?
There are several types of restrictive and malabsorptive operations. Each one carries its own benefits and risks.
Restrictive Operations
Restrictive operations serve only to restrict food intake and do not interfere with the normal digestive process. To perform the surgery, doctors create a small pouch at the top of the stomach where food enters from the esophagus. Initially, the pouch holds about 1 ounce of food and later expands to 2-3 ounces. The lower outlet of the pouch usually has a diameter of only about 3/4 inch. This small outlet delays the emptying of food from the pouch and causes a feeling of fullness.
As a result of this surgery, most people lose the ability to eat large amounts of food at one time. After an operation, the person usually can eat only 3/4 to 1 cup of food without discomfort or nausea. Also, food has to be well chewed.
Restrictive operations for obesity include laparoscopic adjustable gastric banding (LAGB) and vertical banded gastroplasty (VBG).
The Sleeve Gastrectomy is considered a restrictive and metabolic procedure. Performed laparoscopically, two-thirds of the stomach is cut away and removed, leaving a narrow, banana-shaped stomach. The new smaller stomach provides restriction and aids in portion control. The portion of the stomach removed releases a hormone called ghrelin, which is an appetite stimulant. By removing that part of the stomach, there is less ghrelin production. In addition, the portion removed is very distensible-it can stretch very easily and may also contribute to our ability to eat large portions.
The sleeve gastrectomy is not reversible, but with time and if a person frequently overeats, they may stretch their sleeve resulting in less restriction. It will never stretch back to the original size, but may stretch enough to lose your restrictive control.
Although the sleeve gastrectomy is a newer procedure, it has been performed for many decades in combination with the biliopancreatic diversion (BPD). The BPD is a malabsorptive operation where most of the intestine is bypassed. The weight loss is dependent on not absorbing the food eaten and may result in severe nutritional deficiencies. This operation is often reserved for people who need to lose several hundreds of pounds, but these are also the same people who are very high risk for complications because of their larger BMIs. In order to minimize the complication rates, the biliopancreatic diversion was done in stages. The first stage was the sleeve gastrectomy. After the patient lost one hundred pounds, they then went onto the second stage which was most often the biliopancreatic diversion or less frequently, the gastric bypass. What was discovered was that several patients lost a significant amount of weight with the sleeve gastrectomy alone, and did not need to have the second stage of the surgery performed. That is how we have come to do the sleeve gastrectomy by itself. For those patients that do not lose enough weight with the sleeve alone, it would still be possible to perform the gastric bypass (which provides enough malabsorption without excessive malnutrition).
Weight loss with sleeve is gradual, but still at a faster rate than with the adjustable gastric band. Expected excess weight loss is about 60 % at 1 year. Although 5-year data supporting the sleeve is good, the long term data is not yet available.
- Much smaller stomach thus providing great restriction in food intake
- Marked reduction in “ghrelin” production, thus providing a metabolic benefit by reducing hunger
- Encourages weight loss by restriction and some metabolic benefit
- No alteration of the gastro-intestinal continuity thus no malabsorption
- No “dumping syndrome”
- This procedure is considered permanent and irreversible since a portion of the stomach is removed.
- It is considered to be more invasive and thus chances of complications are higher. Nevertheless, this procedure is considered very safe and rarely causes major problems.
- Data on results and long term effects of this procedure is available for less than 10 years. Nevertheless, we do not anticipate any major problems for someone losing most of their stomach as we perform similar procedures for other problems such as cancer and ulcer disease with minimal long term Sequa lea.
Any operative procedure can cause complications. In general the morbidly obese population is at higher risk for worse outcomes with any complication. Thus we go to great measures to provide you with a complete work up before surgery to minimize these risks. Additionally, you should be reassured that programs such as ours with “Center of Excellence” designation are in general considered safer because of much higher standards to which we adhere.
After sleeve Gastrectomy some patients BUT NOT very commonly, may develop severe heartburn that is not controllable with medication. In severe cases surgical intervention may be necessary to correct this problem.
The biggest complication that may occur after sleeve Gastrectomy is a leak. We take great measures to prevent leaks but in rare instances it may occur. It will require surgical intervention most often and if it is untreated it can be life threatening. Fortunately it is very rare.
The laparoscopic adjustable gastric band is a purely restrictive procedure. It involves placing a silastic (plastic) band around the top portion of the stomach so that the stomach acts as if it has been reduced in size. After eating a small amount of food, this smaller stomach becomes distended and the patient feels full. Also, the food passes slower into the remainder of the stomach so that fullness last longer than before surgery. The goal is portion control. The band “tightness” around the stomach is adjustable by adding or removing fluid from a balloon on the inside of the band. This is done utilizing a “port” that is connected to the balloon. The port lies on the abdominal wall, under the skin. The adjustments are performed in the bariatric office, and do not require another operation to perform. No part of the stomach or intestines are cut or divided in order to place the band.
Key Features of the Laparoscopic Banding System
- Stomach “pouch” – is 1-2 ounces in size, fills quickly, and gives the feeling of satiety/fullness. Patients should stop eating when they feel full
- “Stoma” – is the outlet of the band placed around the stomach. This is adjusted by inflating or deflating the balloon. The size of the stoma will determine the rate of weight loss.
- “Port” – is the access port placed under the skin. It can be injected with sterile water or saline to inflate or deflate the balloon in the band to control the weight loss. This can be performed in the office without anesthesia.
Advantages of Lap Banding
- Lower risk of mortality and complications
- No alteration of normal intestinal anatomy.
- It can be adjusted to the individual patient’s weight loss needs.
- Lower risk of long term malnutrition.
- Potentially reversible
Disadvantages of Lap Banding
- Slower weight loss
- Requires closer follow ups and frequent adjustments early on.
- Long term results on implantable devices not available, and the patient could need additional surgery to revise, change or remove the implant
- Needs complete compliance and discipline for patients to be successful.
- Need to alter eating habits for successful weight loss as well as chew food very well to avoid food “getting stuck” at the band.
Risks and Complications of the Adjustable Gastric Band
As mentioned above, no surgery is without risk. Major risks associated with the band can include infection, bleeding, erosion of the band into the stomach, or slippage of the band on the stomach. Both require a reoperation to fix the problem. In addition, there is a risk of deep vein thrombosis or pulmonary embolus. There may also be minor risks such as leakage at the port site; which can often be taken care of with a minor surgery. Vitamin and protein deficiencies can occur if the diet is not well balanced. If the band is removed for whatever reason, there is a high chance the patient will regain all the weight loss as the restrictive mechanism is now gone.
Vertical Banded Gastroplasty
VBG has been the most common restrictive operation for weight control. As figure 3 illustrates, both a band and staples are used to create a small stomach pouch.
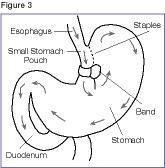
Although restrictive operations lead to weight loss in almost all patients, they are less successful than malabsorptive operations in achieving substantial, long-term weight loss. About 30 percent of those who undergo VBG achieve normal weight, and about 80 percent achieve some degree of weight loss. Some patients regain weight. Others are unable to adjust their eating habits and fail to lose the desired weight. Successful results depend on the patient’s willingness to adopt a long-term plan of healthy eating and regular physical activity.
Restrictive Procedures Weight Loss Related To:
| Surgery Factors | Patient Factors |
|---|---|
| Meal size restriction |
|
A common risk of restrictive operations is vomiting, which is caused when the small stomach is overly stretched by food particles that have not been chewed well. Band slippage, erosion, and saline leakage have been reported after AGB. Risks of VBG include wearing away of the band and breakdown of the staple line. In a small number of cases, stomach juices may leak into the abdomen, requiring an emergency operation. In less than 1 percent of all cases, infection or death from complications may occur.
Combined Procedures (Restrictive & Malabsorptive Operations)
Malabsorptive operations are the most common gastrointestinal surgeries
for weight loss. They restrict both food intake and the number of calories
and nutrients the body absorbs.
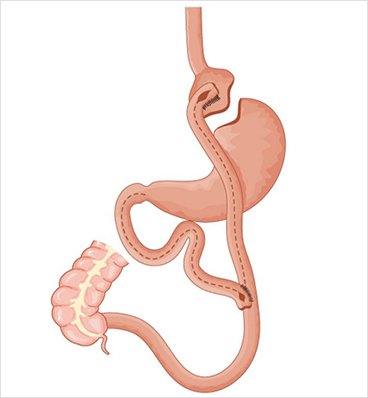
Roux-en-Y Gastric Bypass (RYGB)
The Roux-en Y gastric bypass is a combined RESTRICTIVE and MALABSORPTIVE
procedure. The restriction in this operation is accomplished either by
forming a smaller functional stomach with staples (“short limb”) or taking
out about 66% of the stomach. In either case, the remaining portion of the
stomach is at about 1-4 ounces in size. The size of this new stomach will
start out at about the size of a golf ball (short limb Roux Y gastric
bypass), or small juice glass (long limb Roux Y gastric bypass). Expect
some increase in size as time goes by. We do not put any bands or rings
(foreign materials) around the stomach to make it empty more slowly.
Recall the total length of the intestine varies from 15 to 30 ft. The
malabsorptive component of the operation is achieved by separating the
food from the digestive juices. The “Roux limb” carries the food (~ 2-3
ft) and the digestive juices are carried in the “Biliopancreatic limb” (~
1ft). When the two limbs are rejoined, the food is able to mix with the
digestive juices, allowing the breakdown and absorption of food in the
remainder of the intestine called the “common channel.”
RYGB Weight Loss Related To:
| Surgery Factors | Patient Factors |
|---|---|
| Meal size restriction | Caloric intake |
| Some malabsorption Decreased appetite |
Caloric expenditure |
In review, following gastric bypass surgery, when you eat food, it will go
into the smaller stomach (gastric pouch). The food then enters the route
of intestine referred to as the “Roux limb.” (The Roux limb is also called
the “alimentary limb” because it carries the food). The portion of the
bowel that is not carrying food (biliopancreatic limb) carries the bile
and digestive juices from the liver and pancreas. Full digestion will take
place in the “common channel” where the digestive juice and bile mix with
food. “Short” versus “long” limb gastric bypasses refers to the length of
the bypassed bowel, with the long limb bypassing a greater length of the
bowel, and thus providing more malabsorption.
- The stomach is 1-2 ounces in size in the short limb procedure. It is 12-15 ounces in the long limb bypass. This is the restrictive part of the procedure. It will gradually enlarge in size.
- The intestinal re-routing is the malabsorptive component of the operation. The digestive juices from the liver (bile) and pancreas mix with the foodstuffs (nutrients) farther along the intestines, thus limiting the quantity and type of fats and carbohydrates absorbed.
- The alimentary limb/Roux limb (the new portion of small bowel connecting to the new stomach pouch) transports the food to the “common channel” where it mixes with bile and pancreatic digestive enzymes for the process of digestion to begin. This is measured usually 100-150 cm in length.
- The biliopancreatic limb (the portion of the small bowel which carries bile and pancreatic digestive juices from the “old” stomach to the “common channel”) transports the digestive juices to the common channel to facilitate the digestion of food.
- The common channel area (the last portion of the alimentary limb after the biliopancreatic limb is attached) is the only place you have full digestion. The length of the common channel will determine the degree of malabsorption which may occur after surgery. In particular, fats are NOT absorbed well. This means that ALL of the fat soluble vitamins (A, D, E, and K) are not absorbed well and may have to be taken the rest of your life or metabolic complications will result. In addition, some medicines (if they are fat based) may not be absorbed well. Other elements such as zinc, iron, and vitamin B12 also will not be absorbed well in the long term.
- Long term track record of follow up is available (>30 years).
- Rapid initial weight loss.
- Ensures weight loss by means of restriction and malabsorption, thus ensuring a higher success rate.
- The invasive nature and difficulty of the procedure leads to higher risks of complications and mortality.
- Risk of long term nutritional deficiencies and need for long term supplements.
- Weight loss plateaus after 1 year and the patient may have difficulty continuing to lose weight afterwards if they do not follow a strict diet and exercise program.
- Dumping Syndrome may occur which is a food intolerance to sweets and foods high in fats resulting in abdominal cramps, sweats, palpitations or skipped heartbeats, and diarrhea.
- Procedure is difficult to reverse and is not adjustable.
There are major risks and the potential for complications in any operation (see advantages & disadvantages). This is especially true in the patient who is particularly overweight and in whom there are comorbid factors such as diabetes, heart disease, etc. The risks are further increased in patients who have had prior abdominal operations and especially, prior attempts at weight reduction surgery. These statements are NOT made to scare you but rather to inform you and your family of the potential risks involved in your decision. Fortunately, the overall incidence of complications and morbidity is quite low for patients in our program. It is our intention to minimize your risk by appropriate and judicious patient screening and referral for preoperative specialist evaluation. Remember the adage, “an ounce of prevention is worth a pound of cure,” and accept a referral as being in your best interest.
The list of possible complications after Roux-en-Y gastric bypass include, but are not limited to, bleeding, wound infection, anastomotic leakage, sepsis/peritonitis, deep venous thrombosis, pulmonary embolism, myocardial infarction, pneumonia, and death, as well as long term risks of bowel obstruction, hernias, stomal strictures, pouch dilatation/enlargement, “dumping syndrome”, protein, calcium and vitamin malnutrition, gallstone formation, weight gain, and the need for further surgical interventions.
You should refer to the Informed Consent Sheet for a detailed description of the complications which can occur after weight reduction surgery. It is your responsibility to understand these risks prior to surgery.
Any patient with a Body Mass Index (BMI) equal to or greater than 50 kilograms per meter squared is classified as SUPER MORBIDLY OBESE. These individuals have 2-3 times the risks for surgical weight loss as patients less than 50 kilograms per meter squared.
Patient Testimonials
*All opinions expressed are the sole viewpoint of the individual patient, and as such should not be treated as medical advice. Results will vary for every individual.*
More Success Stories
Frequently Asked Questions
Recovery time can vary, but the typical bariatric surgery patient stays 2-3 days for the laparoscopic gastric bypass and sleeve gastrectomy, and 4-6 days for revisional surgery or the open gastric bypass. The band patients are usually home the same day and do not need to stay overnight.
An exercise regimen is key to maintaining weight loss, and your team at the South Bay Metabolic and Weightloss Institute will help you develop a plan. You’ll start by walking soon as soon as you can after surgery, and continuing to walk more once you go home. Patients with knee or ankle problems are encouraged to swim or bicycle, once cleared by their surgeon.
Patients must stop smoking before any weight loss surgery. Smokers risk having lung problems or infections after surgery. It also slows the healing process. Smoking after surgery can also lead to complications such as ulcers after the bypass or sleeve, or erosion of the band in those patients.
Your doctor and dietician will help you with your specific eating plan, but you can expect to be on a liquid diet right after surgery. After two weeks you can then begin eating pureed or semi-solid food. Most patients resume eating solid food after about four weeks. Again, your doctor and care team will outline your specific diet plan.
National guidelines suggest that bariatric surgery should only be performed on patients 18 years of age or older. Patients should be mature enough to handle the commitment and hard work needed to maintain a healthy lifestyle after surgery.
Each policy is different, though many insurance providers understand that this is a medically necessary and lifesaving procedure. Your team at the South Bay Metabolic and Weightloss Institute will help you to work with your insurance company to determine your bariatric surgery coverage.
If you’re planning to become pregnant, your surgeon will advise you on how long you should wait. Patients are typically told to wait about 18 months, or when your weight loss and nutritional status has stabilized.
No problem. The specialists at the South Bay Metabolic and Weightloss Institute have over 30 years experience with revisions and caring for patients with prior historical procedures/surgeries not performed anymore.
Explore Benefits and Risks
Surgery to produce weight loss is a serious undertaking. Anyone thinking about surgery should understand what the operation involves. Patients and physicians should carefully consider the following benefits and risks:
Benefits*
Right after surgery, most patients lose weight quickly and continue to lose for 18 to 24 months after the procedure. Although most patients regain 5 to 10 percent of the weight they lost, many maintain a long-term weight loss of about 100 pounds.
Co-Morbidities Resolved/Improved
Surgery improves most obesity-related conditions. For example, in one study blood sugar levels of 83 percent of obese patients with diabetes returned to normal after surgery. Nearly all patients whose blood sugar levels did not return to normal were older or had lived with diabetes for a long time.
Risks*
Ten to 20 percent of patients who have weight-loss surgery require follow-up operations to correct complications. Abdominal hernia was the most common complication requiring follow-up surgery, but laparoscopic techniques seem to have solved this problem. Less common complications include breakdown of the staple line and stretched stomach outlets. Blood clots and risk of pulmonary embolism are possible but rare (<1%). Pulmonary embolus is the most common cause of death after bariatric surgery.
Some obese patients who have weight-loss surgery develop gallstones. Gallstones are clumps of cholesterol and other matter that form in the gallbladder. During rapid or substantial weight loss, a person’s risk of developing gallstones increases. Taking supplemental bile salts for the first 6 months after surgery can prevent gallstones. Nearly 30 percent of patients who have weight-loss surgery develop nutritional deficiencies such as anemia, osteoporosis, and metabolic bone disease. These deficiencies usually can be avoided if vitamin and mineral intakes are high enough. Women of childbearing age should avoid pregnancy until their weight becomes stable because rapid weight loss and nutritional deficiencies can harm a developing fetus; this is usually about 2 years.
* Disclaimer: The testimonials, statements, and opinions presented on our website are only applicable to the individuals depicted, and may not be representative of the experience of others. The testimonials are provided voluntarily and are not paid, nor were they provided with free services, or any benefits in exchange for said statements. The testimonials are not indicative of future results or success of any other individuals. Association of South Bay Surgeons a Medical Group, Inc cannot and does not guarantee the medical outcome or the results of individuals utilizing the services provided by us.*










Leave a Reply